Best of CMF Magazine
Recovering Health Services Officer wants to give fellow PTSD sufferers reason to hope
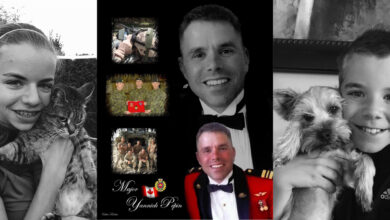
After serving his country for more than 25 years, including two exceptionally challenging tours in Rwanda and Afghanistan, Lt.-Col. Chris Linford is ready to tell the world how he faced down his PTSD demons and won back his quality of life.
In his newly released book Warrior Rising, Chris recalls his career in the Canadian Forces which he began as a drummer in the reserves and later as a nurse and then Health Services Officer in the Regular Force where he helped treat victims in the horrific genocide in Rwanda. Twenty years later he managed the medical care of hundreds of wartime casualties in Afghanistan. He hopes his story will be an education to those uninitiated in the realities of war and a beacon of hope for those who suffer with the daily challenges of post-traumatic stress disorder.
“I decided to write the book because I consider myself a health success story, getting well again after a pretty significant PTSD condition,” says Chris. “I needed to tell the story for veterans who have not yet come forward, for those who are still suffering in silence, those who are at home isolating themselves. I wanted to let them know it can be done; that they need to share their stories. If they`re still in, they need to go to Health Services and ask for help. If they are out of the CF, go see the VAC. It’s not about weakness or being less of a man or a soldier or an officer. It’s about being strong and showing the courage to come forward and ask for help when it’s needed, because life can be so much better when you deal with this issue.”
While awaiting his medical release from the forces at his final posting at Joint Personnel Support Unit (JPSU) in Victoria, B.C., Chris started writing about his PTSD and how the medical services offered by the CF helped him conquer its effects. In 2004, ten years after his tour in Rwanda, his PTSD really hit him.
“Rwanda has become the ‘Oh my God tour’ — You were on that one! I get that a lot. I was probably feeling it for some time but was reluctant to step forward for treatment and was just living with it the best I could. I always had a pretty high degree of coping being a trauma nurse. You just suck it up. And that was the attitude of the forces at the time anyway…just to suck it up and carry on.
“So in 2004, when I was in Borden, I had what you would call a bit of a meltdown and could no longer function either professionally or personally for that matter. I went into year-long treatment with a psychiatrist where they put me on anti-depressants and sleeping meds because I had all but lost my ability to sleep at night. I got better, which was the good news. After about a year I was weaned off the anti-depression medication but I have remained on the sleeping medication ever since 2004, I cannot get off of that.”
Five years later, Chris was deployed to command the main surgical centre at Kandahar Airfield in Afghanistan. Seven months of daily exposure to incoming young soldiers with traumatic injuries from IEDs and firearms, torpedoed the lieutenant colonel back into PTSD hell.
“Afghanistan was the first tour I would do as a non-clinician,” he says. I was more of an administrator and leader of the unit as an executive officer (in Kandahar). So I was responsible for everything that happened from the time the casualty was offloaded from the helicopter to the time they went out at night with the US Air Force to take them to Germany.”
He says the thing that struck him the most was the level of inexperience of the US Navy troops on this mission. Many of them were brand new in the navy and this was literally their first job in their military experience. “They were brand new Navy Corpsmen, that was our equivalent to our medical technicians; they were brand new kids just learning. They were 18, 19, and 20 years old; even younger than my kids at the time. As Deputy Commanding Officer you feel kind of like the Dad to all of these people. The quality of the casualties that were coming in was significantly traumatic and you would have to be blind not to see that it was impacting these young people dramatically. I had done two tours previously (in Kuwait and Rwanda) where I saw a lot of trauma, more trauma than anyone should see. My job in Afghanistan was just to keep an eye on what was going on in the unit.”
His style of leadership is to be right at the front where everything is happening, so he ended up exposing himself once again to an extreme level of trauma cases. “And then having to deal with the kids later who were suffering from what they were seeing. They were learning all of those lessons that I had learned 20 years earlier about dealing with trauma and they were definitely getting quite rattled.”
Surprisingly, he says there was very little turnover on his watch. “And to their credit they all wanted to hang on. They became a very tight unit. That’s what happens in a unit that experiences so much trauma or has so much negative stuff happening to it, it usually binds them even tighter. Of the 250 troops we had working there, we probably only lost three over the entire seven months and that was not due to difficulty dealing with trauma but was for other unrelated issues. So I would suspect that just like when I was their age and exposed to that level of trauma, it didn’t bother me immediately either. It didn’t cause me to have to leave a deployment or anything like that. It didn’t strike me until years later. So what I expect is that these young people will continue in their military careers and then at some point in the future if they don’t deal with the fact that they have been exposed to that level of trauma they could become ill with PTSD.” Through his book, Warrior Rising, Lt.-Col. Linford hopes to motivate some of these soldiers to reach out for help.
“Half way through my deployment in Afghanistan, my PTSD started to come back again and I was going to need more treatment and therapy after the tour. I began to lose sleep again so I spoke with a doctor who helped me out with more medication. It was pretty devastating for me because that was a signal I was going to become ill with PTSD again. I was right in the middle of this very intense mission where a lot of people were counting on me and if I was unable to sleep I would only be able to last so long. I ended up doubling and tripling my sleep meds to get four or five hours sleep a night. We were working seven days a week, 16 to 18 hours a day so I was basically a walking zombie by the time I came home.”
Before his mission in Afghanistan and as CO of 1 Field Ambulance, Chris explains that his whole focus was on getting his troops battle ready. He didn’t have time to think about what the mission might mean for him. One Brigade was on training for this war; getting troops ready for battle was the name of the game. The Med Techs who were going to be working outside the wire, by far the most dangerous part of the mission, needed the vast majority of the effort in training. I spent all my time ensuring that they were well prepared, battle ready and focused on coming back alive. “Unfortunately I did end up losing 2 Med Techs during my time as CO.”
Another casualty for Chris was his belief in the mission. Seeing so much human carnage from their military efforts was more than the Canadian officer could handle.
“I have to say the biggest change for me was my rising level of cynicism for the mission. I was seeing the price that NATO was paying on a daily basis either through death or incredibly life changing injuries happening to young people. I began to question: What the hell were we doing there? The price seemed so incredibly high and from what I could tell, I was seeing very little appreciation from the Afghan people. There seemed to be very little intent on their part to change what was happening in their lives; to change life in Afghanistan for the better. So that didn’t help.”
By Jill Kruse